Selective Serotonin Reuptake Inhibitors (SSRIs) and risk of suicidality
Selective serotonin reuptake inhibitors (SSRIs) are used for the treatment of depression, anxiety and other mood disorders. The locally registered SSRIs include escitalopram, fluoxetine, fluvoxamine, paroxetine and sertraline. They are mostly indicated for patients aged 18 years and above. Fluvoxamine is approved for use in children aged 8 years and above for the treatment of obsessive-compulsive disorder (OCD). Although none of the registered SSRIs are approved specifically for the treatment of depression in children and adolescents below 18 years old, they are used off-label in this patient population. Depression and other psychiatric disorders in children and adolescents can have significant consequences if not appropriately treated. The off-label use of SSRIs is supported by clinical guidelines.1, 2
SSRI-associated suicidality
SSRIs are known to be associated with an age-dependent risk of suicidality, where an increased risk is observed particularly in patients less than 25 years of age. However, the causal association remains to be conclusively established, as the risk of suicidality may be confounded by the patient’s underlying psychiatric condition and its severity. A meta-analysis of 24 short-term placebo-controlled trials of major depressive disorder (MDD) or other psychiatric disorders involving over 4,400 children and adolescents found a greater risk of suicidal ideation and behaviour (but not completed suicide) during the first few weeks after treatment initiation with SSRIs as compared with placebo (4% vs 2%; risk ratio 1.95, 95% confidence interval [CI] 1.28 to 2.98).3 Similarly, another pooled analysis of 295 short-term (median duration 2 months) placebo-controlled trials of 11 antidepressant drugs, of which the majority were SSRIs, in over 77,000 adults with MDD or other psychiatric disorders found a higher risk of suicidal behaviour associated with antidepressant use among patients less than 25 years old (odds ratio [OR] 2.30, 95% CI 1.04 to 5.09).4 However, no increased risk was observed in adults aged 25 to 64 years (OR 1.03, 95% CI 0.68-1.58) and a risk reduction was observed in adults aged 65 years old or greater (OR 0.06, 95% CI 0.01-0.58).
Local prescribing trends of SSRIs
Based on data from the electronic medical records, an average of 50,000 patients were prescribed SSRIs annually between 2017 and 2021. Of these patients, the majority were adults (≥25 years of age; 82.9%), followed by young adults (18-24 years; 13.5%) and children/adolescents (<18 years; 3.6%).
Over those five years, an increasing trend in the prescriptions of SSRIs was observed. The increase ranged from 3.5% to 4.7% year-on-year from 2017 to 2020, followed by a bigger jump of 9.1% from 2020 to 2021. When analysed by age group, the annual proportion of children or adolescents prescribed SSRIs was stable at around 3.4% from 2017 to 2020 and increased to 4.1% in 2021, while those of young adults steadily increased over the years from 11.2% in 2017 to 15.5% in 2021 (Figure 1). In contrast, there was a downward trend in the annual proportion of adults prescribed SSRIs from 85.4% in 2017 to 80.5% in 2021.
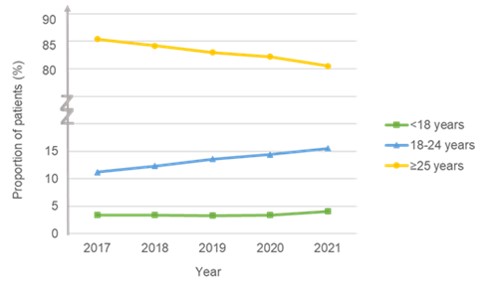
Figure 1. Trend in proportion of patients prescribed SSRIs by age group
Local educational materials for patients
Patient educational materials on SSRIs are available on publicly accessible platforms, including the Medication Information Leaflets (MILs) on HealthHub.5 These MILs, which were developed by the National Medication Information Workgroup* with consensus from the College of Psychiatrists as well as the relevant chapter specialties of the College of Physicians, provide a brief overview on the uses of SSRIs and their side effects. The warnings on suicidality and mental state worsening in these MILs have recently been strengthened to highlight such risks in young people aged below 25 years and to improve patient awareness and education.
HSA’s assessment and advisory
HSA, in consultation with its Product Vigilance Advisory Committee, has assessed that while warnings and advisories pertaining to suicidality risk have been highlighted in the local package inserts of SSRIs and patient educational materials, it would be relevant to remind healthcare professionals of SSRI-associated suicidality in young adults and the availability of MILs to aid patient counselling. This is in view of the increase in the use of SSRIs locally.
Healthcare professionals are encouraged to refer to the available MILs on SSRIs during medication counselling to their patients and/or caregivers. This is to facilitate the communication of SSRI use and their side effects.
*This workgroup comprises cluster partners (National Healthcare Group, National University Health System and SingHealth), community pharmacies (Guardian, Unity and Watsons) and the Pharmaceutical Society of Singapore
References
- https://www.ranzcp.org/files/resources/college_statements/practice_guidelines/clinical_guidance_on_the_use_of_antidepressant_med.aspx
- https://www.nice.org.uk/guidance/ng134
- https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/suicidality-children-and-adolescents-being-treated-antidepressant-medications
- BMJ. 2009;339:b2880
- https://www.healthhub.sg/a-z/a?cat=medications
Healthcare professional, Industry member, Therapeutic Products
Published:
Safety Alerts